Denial Prevention
Faster claim management. Financial success. Less stress.


We’re Here to Advocate for You
What is Denial Prevention?
Denied claims create costly delays and administrative burden – but with TMC, you’re not facing them alone. Our Denial Prevention & Management services are built into every therapy partnership, helping you avoid issues before they start and resolve them efficiently when they do.
From navigating audits and responding to ADRs to managing appeals and tracking trends, our team works side by side with your billing and therapy departments to protect earned revenue and reduce disruption. We stay ahead of CMS and payer requirements so your staff can stay focused on care, and not paperwork.
Prevention & Resolution
When denials happen, TMC takes the lead. Our team manages the entire appeals process - from gathering documentation and preparing responses to submitting directly to payers. We act quickly, communicate clearly, and handle the follow-through, so your billing and clinical teams don’t have to. It’s hands-on support that removes the hassle, protects your reimbursement, and gives you peace of mind.
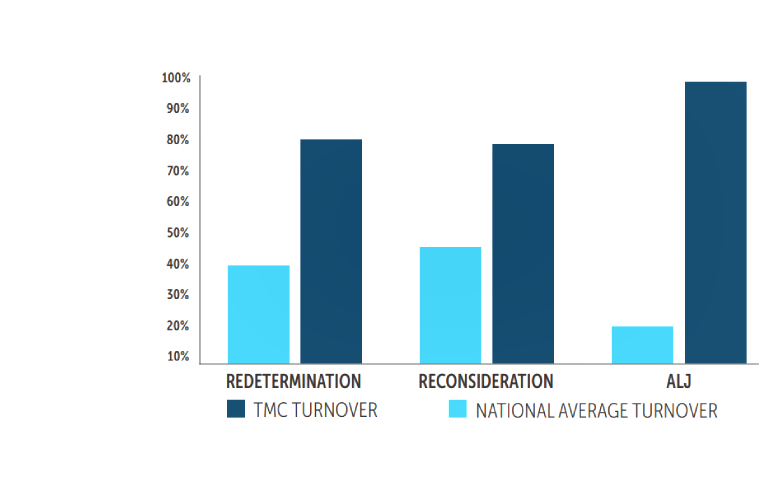
Results You Can Rely On.

Brandon, Assistant Manager -
From day one, TMC has invested in my professional growth and taken an active interest in my personal growth. I am a better clinician because of the resources offered.

Christina, LPN, MNCM -
TMC is a well-organized company that seems to have its patients and clients at the forefront. They go above and beyond for the residents under their care.

VP of Special Services - Skilled Nursing Facility Chain
What a long-term care provider needs from a rehab vendor are quality care expertise, appropriate staffing, regulatory knowledge, and a partnership. TMC provides all that and more.